Cut the Salt: The Need to Re-Classify Sodium as an Additive in the United States
by Kate Klein, MPH candidate
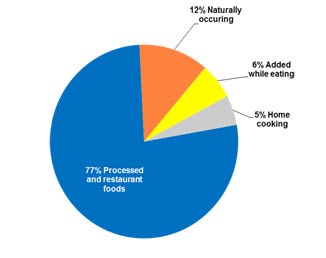
How many of you started your day by eating a breakfast cereal, a bagel, toast, or a muffin? Of course you realized that in those foods you were consuming as much sodium as you would find in a bag of chips? No? Not surprising. Many of the seemingly benign foods that we eat today have way more sodium than they really need. In fact, most of the sodium in the typical American diet is not from the foods we might classify as extremely salty, like pretzels, french fries and potato chips. In the US diet, 77% of sodium comes from processed and restaurant foods, 12% occurs naturally in foods, 6% is added at the table, and 5% is added during cooking.
The Dietary Guidelines for America state that persons two years and older should have a maximum of 2,300 mg per day, though preferably they should consume 1,500 mg per day[i]. People over 50 years old or with existing conditions should have even less. The startling fact is that most Americans consume fifty percent more than that, ingesting an average of 3,400 mg per day[ii]. Americans’ salt consumption has been shaped in part by changes in eating habits as people consume more processed foods, dine out more frequently, and prepare fewer meals at home. Additionally, Americans have grown accustomed to saltier foods as the amount of salt in the nation’s food supply has increased over time.
Throughout the world, there is growing concern about increased rates of high blood pressure, cardiovascular disease, heart attack, stroke, and diabetes. Since the 1970’s doctors and advocates have been making the case that, in the United States, the sodium levels in packaged grocery items and restaurant foods are much higher than they need to be. This problem is not exclusive to the US. Japan, Finland, and the UK, among others, have already instituted successful sodium reduction campaigns. The US has been trying for 40 plus years, and the time is now to make a change for the benefit of our citizens.
The National Salt Reduction Initiative (NSRI), spearheaded by the New York City Department of Public Health, is concerned that consumers lack a choice when it comes to regulating sodium in their diet. As such they want to see policy that will reclassify sodium as an additive, revoking its current status as a ‘generally recognizable as safe’ (GRAS) food. This would allow the FDA to regulate the acceptable levels of sodium in packaged and restaurant foods. They would also like the percentage of Daily Value for sodium to be reduced, from 2,300 milligrams per day to 1,500 milligrams per day. They want to encourage the public to keep their consumption at the safe level of 1,500 mg per day, rather than assuming the maximum, as it is currently listed, is how much they should consume.
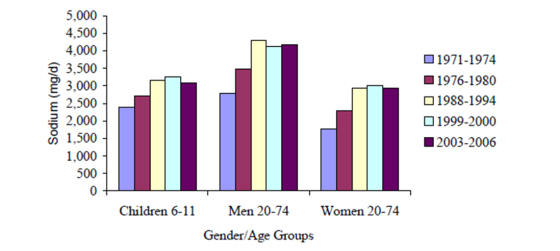
Mean daily sodium intake (in mg) for the U.S. population, 1971 to 2000
Source: Briefel and Johnson (2004) and NHANES (2003-2006)
The National Salt Reduction Initiative (NSRI) is a coalition that includes 70 cities, states and national health organizations. The goal of the NSRI is to reduce Americans’ salt intake by 20% over five years[iii]. Currently, the initiative is focusing on education and voluntary reductions by packaged food manufacturers and the restaurant industry. They have developed targets to guide company reductions in the salt levels in 62 packaged food categories and 25 restaurant food categories. The initiative includes voluntary two and four year targets for average salt levels in each category of food. Currently, 27 large packaged food manufacturers and 6 major restaurant chains have signed on to work on reducing salt in their products. To see those companies, click here.
The NSRI will be tracking those companies progress by monitoring sodium in the food supply and keeping in constant contact with cooperating manufacturers and restaurants to make sure they are keeping their commitment. Information from the Centers for Disease Control’s National Health and Nutrition Examination Survey (NHANES) will be used to track the public’s sodium intake. The NSRI began their work in 2009 by setting their target limits. While monitoring interim progress, they will evaluate their achievements this year.
The health implications are clear. Reducing American’s sodium intake is imperative to reducing the rates of many of the major health problems we see today. Doctors representing the American Public Health Association (APHA) have estimated that sodium reduction would save 150,000 lives a year from strokes, heart attacks and other related illnesses.
Advocates for sodium reduction have varied estimates on the financial savings that implementing this policy will provide. The Harvard School of Public Health conservatively estimates a savings of $18 billion dollars in health care costs each year[iv]. Researchers at Heart.org go on to estimate another $32 billion dollars in savings for improved quality of life. This would make for a combined savings of $50 billion dollars per year[v].
The administrative implications of reclassifying sodium as an additive are that a coordinated effort between the Food and Drug Administration, Health and Human Services, and the Department of Agriculture will need to be organized as the transition takes place. This should not be difficult, as there are many other areas in which these branches work together. Outside of that, the policy will also require that state and city public health departments add educational components to their programs. Additionally, there will need to add an oversight component to make sure food manufacturing companies and restaurants are in compliance with the new policies.
Reclassifying sodium as an additive and removing it from the GRAS list is a legal & political process that is already being contested. Lobbying organizations such as The Salt Institute are expounding the benefits of salt and ignoring it’s over use and the resulting health problems associated with it. Steps have already been taken to push for this policy change. In 2008, the Senate and the Assembly of the State of California, jointly, with the Legislature of the State of California passed a resolution to urge the FDA to reclassify sodium as an additive, thus revoking its GRAS status[vi]. They also urged the Department of Agriculture and Health and Human Services to set new food guidelines, reducing the levels of sodium recommended for daily intake. In 2011, the FDA and the Department of Agriculture’s Food Safety and Inspection Service (FSIS) solicited public comments on approaches to reducing sodium consumption. The AMA, as part of the NSRI, submitted a letter encouraging the FDA to support the reclassification. The FDA seems to still be considering these recommendations[vii].
When we talk about implementation, a concern from the packaged food and restaurant industry is that reducing salt levels will make their foods no longer taste as good to their consumers, who will then seek out other foods will the levels of sodium they are used to. A way to tackle that would be to implement these changes in a gradual manner, such that the general public would not notice a dramatic difference. A five or ten year plan could be made to incrementally reduce the amount of sodium in food to the new maximum levels, which will be determined by the public health community. Much of the work already being done by the NSRI will pave the way for these standards. Additionally, the US may look to success stories like Finland and the United Kingdom, who made great strides in reducing sodium consumption in their countries, rather than trying to reinvent the wheel. To read more about other countries initiatives, click here. These changes will make a huge impact in the overall health of our public in the long term, and done systematically, are actually relatively easy to do.
References:
[i] http://www.health.gov/dietaryguidelines/
[iii] http://www.nyc.gov/html/doh/downloads/pdf/cardio/cardio-salt-nsri-faq.pdf
[iv] Briefel, R and Johnson, C. Annual Review of Nutrition Vol. 24: 401-431 (July 2004) “Secular Trends in Dietary Intake in the United States.”
[v] Nainggolan, Lisa. TheHeart.org, (2009). “Cutting salt intake in US could save $50 billion a year.” http://www.theheart.org/article/1004085.do
[vi] California Legislative Council Digest, Bill number SJR 28. http://www.leginfo.ca.gov/pub/07-08/bill/sen/sb_0001-0050/sjr_28_bill_20080807_chaptered.html
[vii] Havas, S., Dickinson, B., Wilson, M., Journal of the American Medical Association, p. 1439-1441 (September 2007) “The Urgent Need to Reduce Sodium Consumption.”
Cover Photo by kaboompics via pexels: creative commons


Leave a comment